neck pain shortness of breath
 How Your Neck Pain May Affect Your Breathing
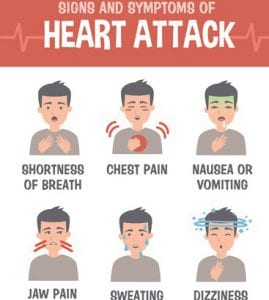
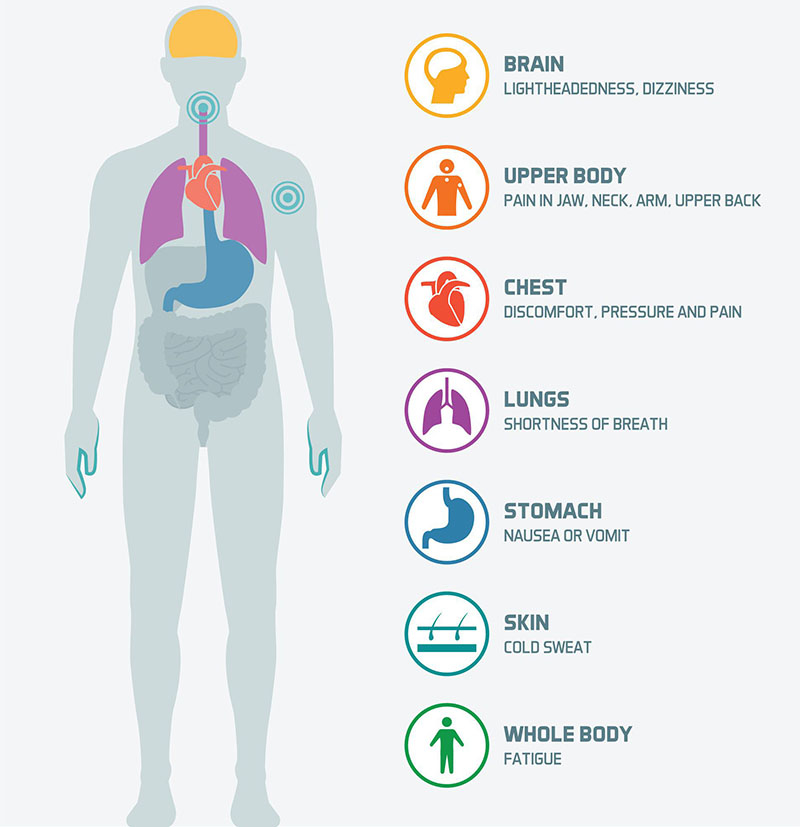
How Your Neck Pain May Affect Your BreathingConditions " Treatments Conditions " Treatments9 Symptoms You should never ignore Pain, fever, lack of breath, when are they a temporary discomfort or something much worse? by Beth Howard, , December 2012/Jan. 2013 Silence Comments: 0 You wake up one morning with a fever. Or maybe you have a bad neck pain. How do you know if a symptom is serious or not? "The things that most worry about doctors are the new symptoms that develop quickly, rather than the things that develop over a long period of time," says Keith L. Black, M.D., president of neurosurgery at Cedars-Sinai Medical Center in Los Angeles. Another warning sign? That feeling that tells you something's not right. "You know your body better," says Len Lichtenfeld, an assistant doctor at the American Cancer Society. "When you see or feel something different or just feel 'off', pay attention; don't dismiss it. "Here are nine symptoms and what they might mean. Getty Images / Background Images Does your symptoms deserve a visit to the hospital?1. Sudden Intense Headache1. Sudden Intense Headache The big worries: If you experience unlike any person you've had before, especially if it rises in seconds to minutes anywhere in your head, you might indicate a broken aneurysm, a blood vessel in your brain that suddenly explodes, requiring immediate attention. The big worries: Also, your doctor will want to rule out three other conditions: Cardiac headacheMeningitis ArteritisTemporal What else could be: Sleeves can cause pain in the forehead before the famous skin reaction (slates is a painful appearance of the herpes zoster virus that is numb in anyone who has had chicken pox). Contrary to common belief, it is unlikely that sudden severe headaches are a sign of a brain tumor. Rather, the research shows that two thirds of patients diagnosed with a brain tumor experienced headaches, deaf pains, pains or pressure, which were constantly worsening over a period of weeks to months. What else could it be:2. Breast pain2. Breast pain Big concerns: Any intense discomfort, heaviness or pressure — like an elephant sitting in the chest — could spell. It can be combined with pain by radiating an arm, nausea and vomiting, sweating and shortness of breath. Women may experience more subtle symptoms, such as fatigue, burning sensation, or upper abdominal pain. Anyway, call 911. "If it's a heart attack, a delay could cause the heart muscle to get damaged," says Eric Topol, M.D., a cardiologist at La Jolla Scripps Clinic, California. If these symptoms occur only during exercise, it may also be angina, which occurs when the heart muscle temporarily does not receive enough blood. Big worries: Acute chest or upper pain (often described as a rivet sensation) can be caused by a tear in the aorta, known as aortic dissection, which requires immediate attention. Fortunately, this condition that threatens life occurs in only three out of 100,000 people. What else could it be: "Perhaps 10 to 20 percent of cases of intense chest pain are due to heart problems but to [GED]," Topol says. Rarely, it could also indicate esophageal spasm, an abnormal contraction of the esophagus muscles, which transports food from the throat to the stomach. Both conditions can be treated with drugs, but it is always prudent to go to the RER: "It is a heart attack or angina until proven otherwise," Topol says. What else could it be:3. Weight loss without explanation3. Unexplained Weight Loss Big Concerns: Losing more than 5 percent of your body weight—without trying—for a six-month period it could mean cancer: Weight loss is a symptom in up to 36 percent of cancers in older people. "If you or a family member suddenly lose weight after trying 400 times before, you have to ask, 'Why is this time the charm?'" says Lichtenfeld. Big worries: What else could it be: Endocrine disorders are a common cause of unintentional weight loss. Of those with endocrine disorder (especially hyperthyroidism, a hyperactive thyroid), up to 11 percent experience weight loss. The condition also triggers concern, sweating, increased appetite and difficulty concentrating. What else could it be:If your weight loss is accompanied by extreme thirst or hunger, fatigue and , it could be a sign of diabetes. Gastrointestinal conditions such as inflammatory bowel disease and celiac disease also cause weight loss, as well as symptoms such as diarrhea and abdominal pain. Depression and other psychiatric conditions can also be blame. "Decreasing appetite and weight loss are very common symptoms of depression," says Susan G. Kornstein, M.D., psychiatry and obstetrics/gynecology professor at the University of Virginia Commonwealth. "But patients with unexplained weight loss must undergo work to rule out general medical causes. "4. Unusual Bleeding4. Unusual Removal Big concerns: Ulcers and colon cancer can cause rectal bleeding or black or tar stools, says Andres Pardo-Agila, a family medicine doctor at the University of Texas Health Sciences Center in Houston. If you haven't had a colonoscopy recently, talk to your doctor. Vaginal bleeding may be related to gynecological cancers. Blood vomiting may result from stomach or esophageal cancer, and people with lung cancer may cough blood. "Whenever you see blood where it shouldn't be, see a doctor," Lichtenfeld says. Big worries: What else could it be: Blood in hemorrhoids may be due to hemorrhoids, while blood in the urine may be the result of a kidney or bladder infection. Long vaginal bleeding after menopause may be due to growth of benign or fibroid polyps. The blood voted may result from a tear in the blood vessels or from an ulcer in the stomach or esophagus. And blood cough can occur with noncancer conditions, such as bronchitis, pneumonia or tuberculosis. "There are many common reasons to see blood where you don't expect it, but it still has to be examined and treated," says Lichtenfeld. What else could it be? High or persistent fever5. High or Persistent Fever Big worries: Fever is the way to fight your body's infection. But "The fever of 103 degrees and above guarantees a journey to the doctor — period," says David Bronson, M.D., president of the American College of Physicians. It may indicate an infection of the urinary tract, pneumonia, endocarditis (inflammation of the lining of the heart chambers and valves) or meningitis, which may require antibiotics to clarify. A low-grade persistent fever—for several weeks—no obvious cause is characteristic of some infections, including sinus infection, and some cancers, such as lymphoma and leukemia. "The cancer is on the list of things we think, but it's usually not the first," says Ronan Factora, M.D., a geriatrician at the Cleveland Clinic in Ohio. Big worries: What else could it be: The fever can be triggered by a virus, which, depending on your health and other symptoms, may require hospitalization. What else could it be:6. Breathlessness6. Breathlessness Great worries: Sudden shortness of breath may indicate a pulmonary embolism when a blood clot is formed in the deep veins of the body (usually in the legs), travels to the lungs and stays in the blood vessels of the lung. I suspect an embolism if you have recently traveled, have been subjected to surgery or have been immobile, and/or your lack of breath is accompanied by chest pain and coughing blood. If you find yourself gassing after going up two or three stairs or getting tired before what you used to do, doctors will want to rule out chronic obstructive pulmonary disease (COPD), especially if it is accompanied by a cough and fatigue and you have a history of smoking. Irregular heart rate, congestive heart failure and other types of heart disease are additional possibilities. When the organs are not getting enough oxygen, inhalation can result. See a doctor, stay. Big worries: What else could it be: Breathlessness can occur with asthma, bronchitis or pneumonia. You may also experience shortness of breath, sometimes with heart palpitations, if you are under extreme emotional distress or anxiety. Regardless, patients should go to the doctor. "It doesn't jump to a psychological problem unless there's nothing else," says Factora. "But we don't want to lose those few cases where survival is at stake. "What else could it be:7. Sudden confusion7. Sudden Confusion Great concerns: If you are experiencing sudden confusion, personality changes, aggression or inability to concentrate, it is important to see a doctor immediately. "The death rate for serious confusion is quite high. You have to figure out what's going on," Bronson says. In the worst case, a brain tumor or a brain bleeding might be behind the delirium. If you are also experiencing a deeply rooted speech, difficulty finding the right words, or numbness or weakness in the face, hand or leg, stroke is a strong possibility. "You have a window of about two to three hours to get to the hospital," says the Black Cedars-Sinai. Beyond that, brain loss can be irreversible. Big concerns: What else could it be: Alcohol-drugs and interactions can also affect your mental state. In addition, confusion may indicate an infection, abnormal blood pressure, low blood sugar or dehydration, each of which should be ruled out by a doctor. What else could be 8? Swelling in the legs 8. Swelling in the legs Big worries: A fluid buildup (called edema) in the limbs can be caused by a number of conditions, but the one that most concerns doctors is heart failure, when the heart cannot pump as much blood as the body needs. When that happens, the blood rests on the veins, causing the fluid to accumulate in the tissues of the body. "The swelling of the legs, especially if it is persistent, should never be ignored," says Gordon F. Tomaselli, director of the cardiology division of Johns Hopkins University School of Medicine in Baltimore. Heart failure is suspected when both legs are affected and the patient also has a lack of breath, fatigue and chest oppression. Big worries: What else could it be: A vein problem known as venous insufficiency can also cause swelling. Normally, the valves in the veins of the legs keep the blood flowing back to the heart, but in those with venous insufficiency, these valves are weakened, causing a backup of the blood. "If the valves are the problem, the swelling usually disappears when it's lying down," Tomaselli says. Compression media can help. Swelling can also result from hypothyroidism (not enough thyroid hormone). What else could it be: 9. Sudden or severe abdominal pain9. Intense or severe abdominal pain Large concerns: Sudden abdominal pain may indicate that an aortic aneurysm - a lump that develops in the aorta, often in the abdominal area - has broken. "If the breakdown of the aneurysm, the pain tends to be sudden and severe and typically centralized around the belly button," says Richard Desi, a doctor, a gastroenterologist at the Mercy Medical Center in Baltimore. Alternatively, sudden pain may indicate a perforated viscous (a hole in the stomach, intestine, or other hollow organ), often due to an ulcer. Intestinal ischemia, which occurs when blood flow to the intestines decreases or stops, oxygen-centred tissues, can also be a culprit. "It's more common in older patients, patients with heart failure or atrial fibrillation," says Brian Putka, a doctor, a gastroenterologist at the Cleveland Clinic. Each of these conditions is life threatening, which requires emergency surgery. The big worries: What else could it be: Abdominal pain is often due to bile stones, which are hard and stony deposits that stay in a gallbladder duct, which leads to acute pain, as well as nausea and vomiting. Diverticulitis — inflammation or infection in small bags of the large intestine — may be another cause of sudden and severe pain, along with changes in bowel habits, fever and nausea. Although irritable bowel syndrome can trigger painful spasms in the colon, the pain tends to come and pass over time and can also cause constipation, diarrhea, or alternate outbreaks of both. Appendicitis is a less likely candidate for sudden abdominal pain in the more than 50 years, as the condition is less common with age. When it occurs, however, it expects to gradually worsen pain in the lower right quadrant of the abdomen. What else could it be: Also of interest Join the discussion Please leave your comment below. You must be logged in to leave a comment. AARP MembershipDiscounts & benefitsAARP is a non-profit organization that empowers people to choose how they live as they age. Members Benefits Disrupt AgingCommunitiesInformation For YouAARP FoundationFor ProfessionalsHealth & WellnessSocial Security & MedicareFamily CaregivingWork & Jobs Take Action Have fun, look, listen You're leaving AARP.org and go to our trusted provider's website. The terms, conditions and policies of the provider apply. Please return to AARP.org to learn more about other benefits. Your email address is confirmed. You will begin receiving the latest news, benefits, events and programs related to AARP's mission to empower people to choose how they live as they age. You can also update your account at any time. You will be asked to register or log in. In the next 24 hours, you will receive an email to confirm your subscription to receive emails related to AARP volunteering. Once you confirm that subscription, you will be regularly receive communications related to AARP volunteering. In the meantime, please feel free. Find ways to make a difference in your community Javascript must be enabled to use this site. Please enable Javascript in your browser and try again.

Chronic Neck Pain and Breathing Problems - How To Help

When to Worry about Shortness of Breath (and When Not To)
Chest Pain: Is it a Heart Attack or Your Spine? - Physio Works...
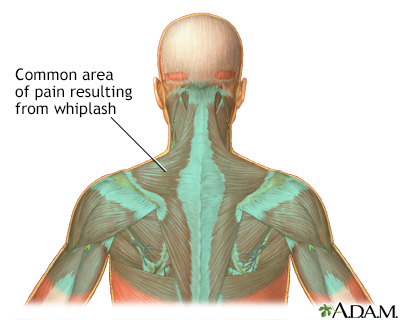
Neck Pain and Breathing Pattern Disorders - Physiopedia
:max_bytes(150000):strip_icc()/right-sided-chest-pain-symptoms-and-possible-causes-4116859-5c77334ec9e77c00012f815f.png)
Causes of Right Side Chest Pain
Neck Pain and Breathing Pattern Disorders - Physiopedia

Heart Attack Neck Pain | Heart Attack Warning Signs
/portrait-of-20s-young-asian-woman-suffering-pain-and-medical-sickness-in-bedroom-at-night--sore-throat--neck-related-pain-symptoms-1253588745-c9c369af88b242dbb691198fdd1f3b4a.jpg)
Panic Attacks and Shortness of Breath
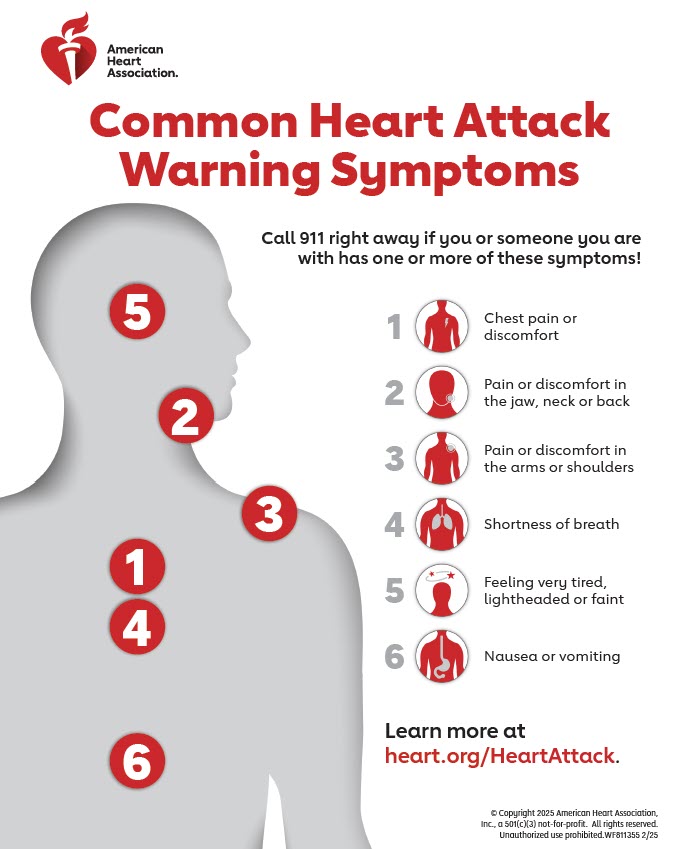
Warning Signs of a Heart Attack | American Heart Association
What Causes Back Pain and Shortness of Breath?

A Visual Guide to a Heart Attack | Signs of heart attack, Heart attack treatment, Heart attack symptoms

Symptoms You Should Never Ignore - Pain, Shortness of Breath

Case 2: Neck Pain, Neck Swelling, and Chest Pain in a 17-year-old Boy | American Academy of Pediatrics
Neck pain Information | Mount Sinai - New York
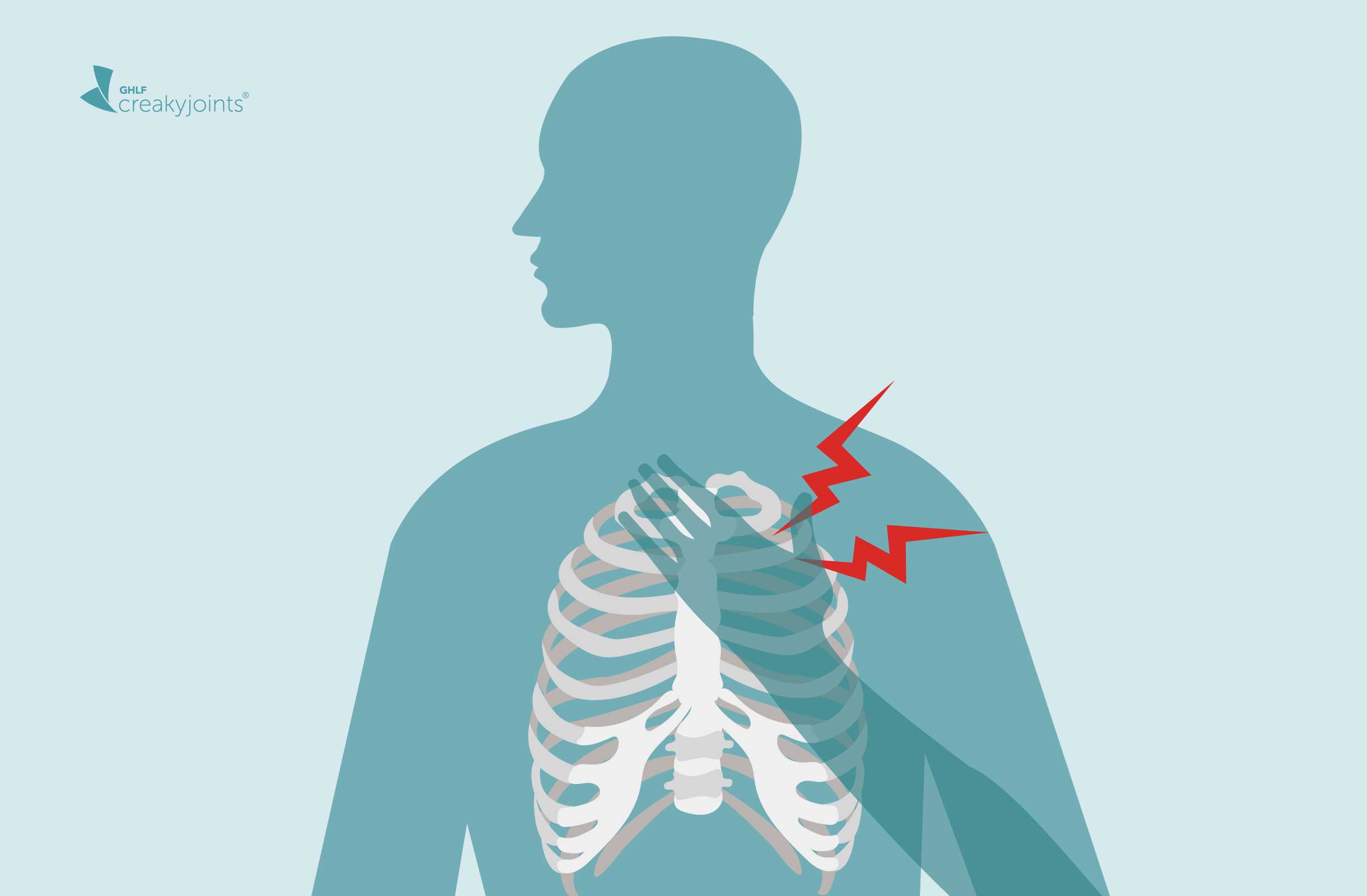
Chest Pain in Fibromyalgia: Causes, Symptoms, Treatment
:max_bytes(150000):strip_icc()/lung-cancer-symptoms-4014389_color-9405196b97064d509fe43ef1f8f14e2d.gif)
Lung Cancer: Signs, Symptoms, and Complications

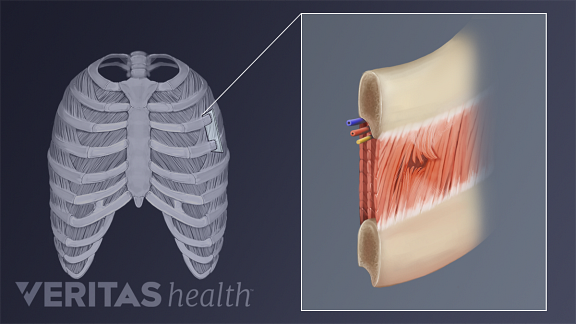
How Scoliosis Affects Rib Pain, Lung Function & Shortness of Breath
Chest pain | healthdirect

C4 root compression leads to phrenic nerve palsy with shortness of breath, chest pain, and elevated hemidiaphragm - The Lancet
:max_bytes(150000):strip_icc()/shoulder-pain-and-lung-cancer-2249407-01-5b854f80c9e77c0050771415.png)
When Might Shoulder Pain Be a Sign of Lung Cancer or Mesothelioma?

Chest Pain: Is It Anxiety, a Heart Attack, or COVID-19?

Pain in neck shoulders head; nausea short of breath other symptoms? - Migraine

Can cervical spine instability cause heart palpitations and blood pressure problems? – Caring Medical Florida

Chest pain: 26 causes, symptoms, and when to see a doctor

Shortness of Breath | Circulation

Chest and Shoulder Pain: Symptoms, Causes, and Diagnosis

Neck Pain and Breathing Pattern Disorders - Physiopedia

Acid reflux and shortness of breath

Can cervical spine instability cause heart palpitations and blood pressure problems? – Caring Medical Florida
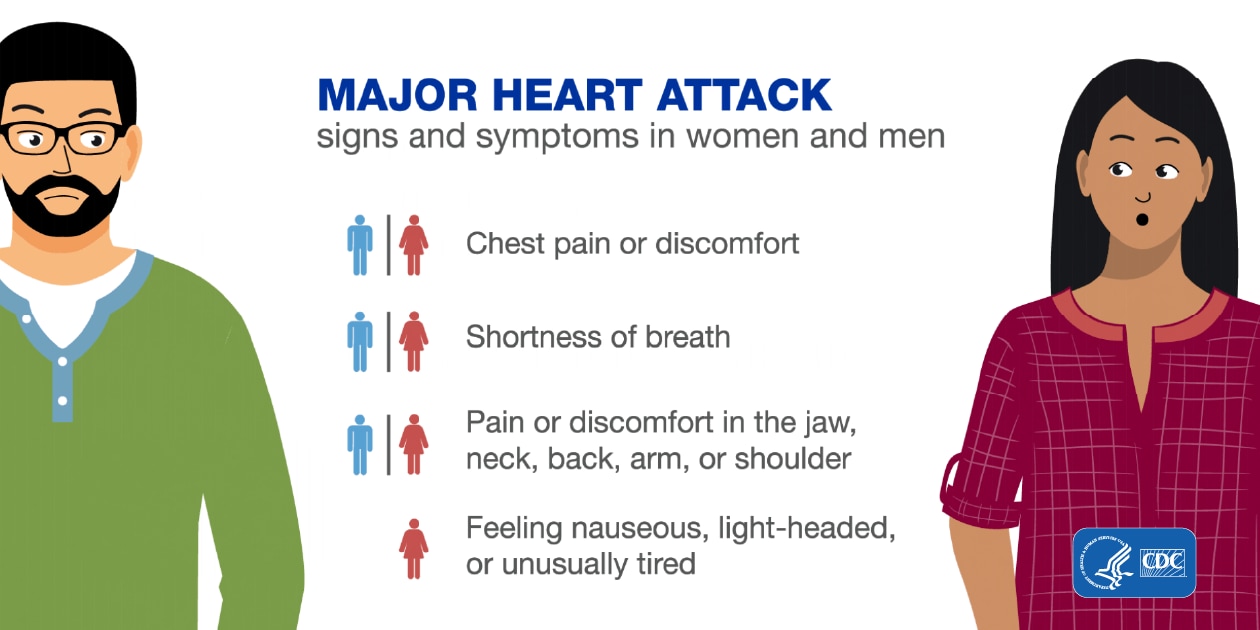
Heart Attack Symptoms, Risk, and Recovery | cdc.gov

Could My Symptoms Be Covid-19? - The New York Times

Medical mystery: What caused chest pain, shortness of breath in older man?

Back Pain When Breathing: Causes, Symptoms, Treatment

Understanding Apical Breathing: Headaches, Neck Pain, & Shortness of Breath | Burnaby RMT | Absolute PhysioCare

Pain in Right Side of Chest: 15 Causes
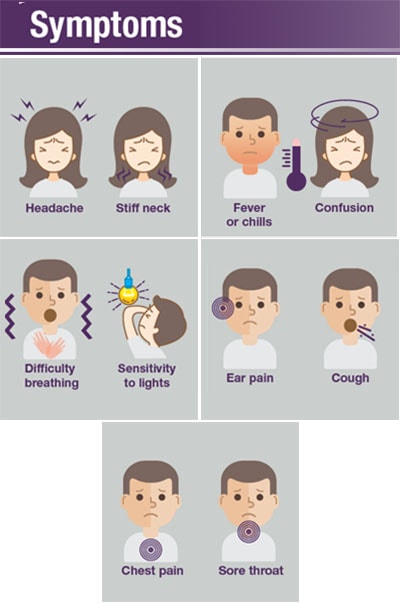
Pneumococcal Disease | Symptoms and Complications | CDC

Could My Symptoms Be Covid-19? - The New York Times
/thyroid-cancer-symptoms-5b4e0b94c9e77c003ec22798.png)
Thyroid Cancer: Signs, Symptoms, and Complications
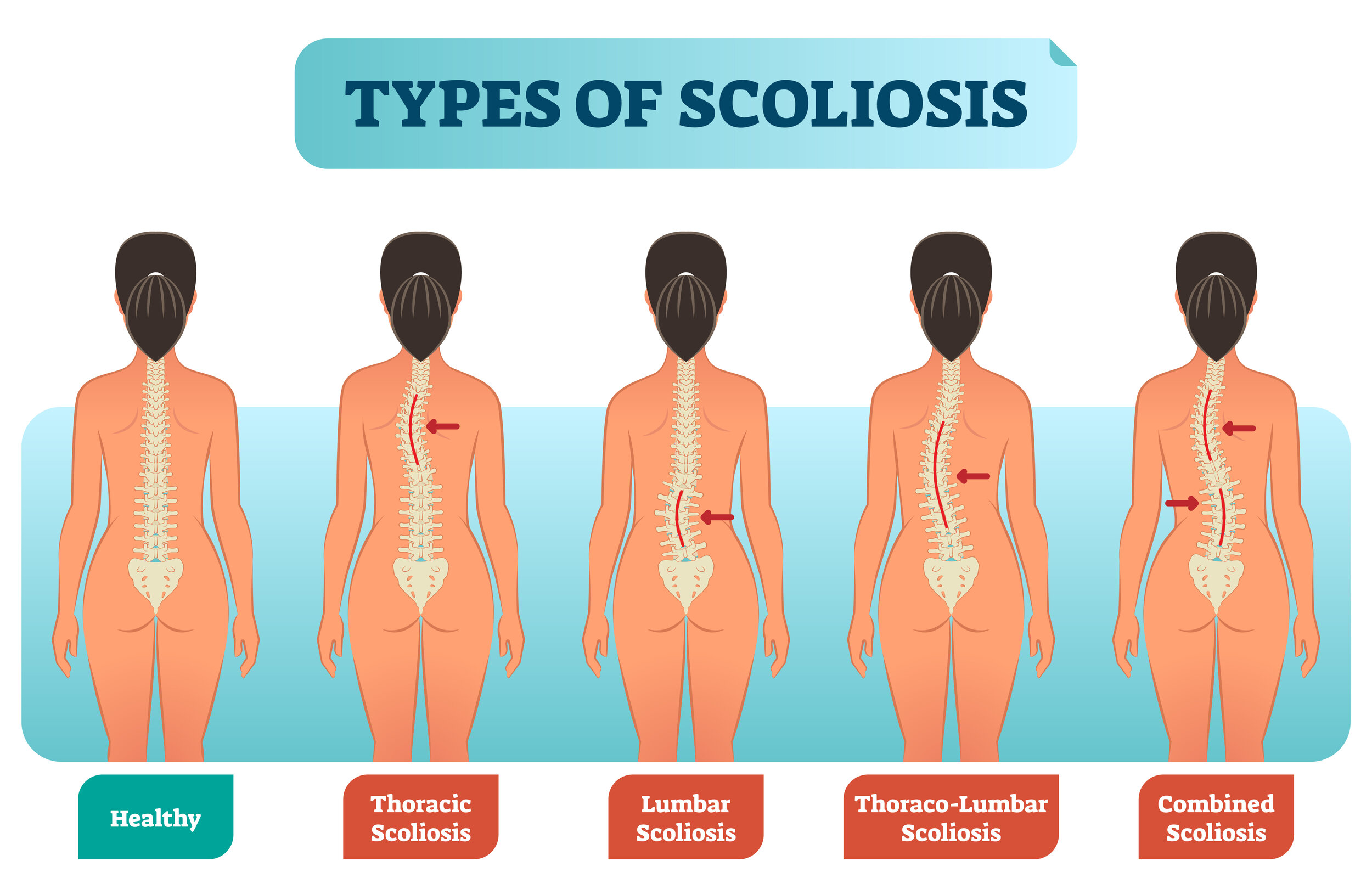
How Scoliosis Can Lead to Breath Shortness
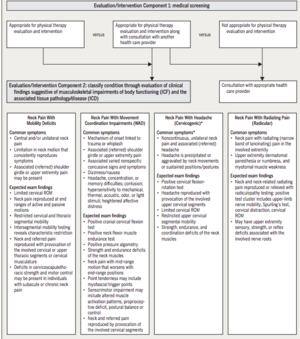
Neck Pain and Breathing Pattern Disorders - Physiopedia
Posting Komentar untuk "neck pain shortness of breath"